Disaster Medicine: Having the knowledge is essential; the ability to share is crucial
Ayman Jundi shares what drew him to the field of emergency and disaster medicine and what has prompted him – and the University of Central Lancashire (UCLan) – to launch its ground-breaking master’s course in Disaster Medicine this year.
UCLan's brand new Master's course in Disaster Medicine is planned to launch in September 2020. The course will offer an exciting opportunity for interested healthcare professionals to develop the required knowledge and skills to be part of a medical relief response in case of a disaster. Image: Valerii Minhirov/123rf
On the face of it, I have been working in Emergency Medicine for 27 years. In reality, my involvement in this fascinating discipline dates back a further decade – back to my time at the American University Hospital in Beirut in the early 1980s. I was supposed to be a surgical trainee, with the intention of going for specialist training in Neurosurgery. Somehow, I always found myself in the Emergency Room (ER) of Beirut’s most prestigious teaching hospital.
The Lebanese Civil War was at its fiercest and most vicious phase, and the American University Hospital ER, at that time the largest Trauma Centre in the Middle East, was where large numbers of civilian casualties, as well as quite a few armed fighters, ended up when they needed emergency treatment.
My passion for Emergency Medicine grew almost uncontrollably, and I could not stay away. I became increasingly involved in the assessment and management of trauma and war injuries, as well as ‘medical’ emergencies that presented to the ER. Eventually, the most obvious decision was finally visible to me: Emergency Medicine was the career path for me.
I was regularly exposed to the challenges of managing mass casualties in an environment and a system that was ill-prepared for them. Don’t get me wrong: the American University Hospital was a highly regarded, well-funded, state-of-the-art academic and clinical establishment that followed the most up-to-date guidelines and protocols of diagnosis and treatment. However, the concepts of ‘Major Incident Management’ and ‘Disaster Management’ were not in anyone’s thoughts. The concept of triage did not exist, and all the essential current considerations for the management of mass casualties that we now take for granted had not been thought of in 1980s Beirut.
Fast-forward to January 2000. Now a Consultant in Emergency Medicine at Lancashire Teaching Hospitals, my specialist interests include Mass Casualties and Major Incident Management in addition to Resuscitation Training and Medical Education. I have been given the task of writing the Major Incident Plans for the newly merged Trust, and I have been heavily involved in the training of hospital staff in the implementation of these plans. I honestly believe that, subconsciously, my experience in dealing with mass casualties with no system to support that operation has been the subliminal drive for me to ensure that in my current position, we have the best opportunity to do the best we can for those casualties, by ensuring that efficient systems are in place and that staff are properly trained to use them.
Another fast-forward to March 2011. The peaceful, popular uprising that started in Syria, my country of birth, has encountered a violent and massively disproportionate response from the authorities and the conflict was rapidly turning into a comprehensive assault on civilian communities that have arisen against a tyrannical dictatorship.
From the very early days of the uprising, it was clear that healthcare in Syria was going to need substantial support, for several reasons. To start with, the violent and indiscriminate response against unarmed and unprotected civilian populations will invariably mean significant numbers of casualties. These casualties will be forced to utilise an overstretched, poorly equipped and poorly staffed healthcare system. Furthermore, they will have war injuries that the doctors and nurses in Syria are manifestly unfamiliar with and have little or no experience in treating.
And to compound all these hurdles, there has been distressing but confirmed and recurrent reports that healthcare infrastructure and healthcare staff were being deliberately targeted by airstrikes and shelling.
A number of healthcare professionals of Syrian descent working and living in the UK, US and Europe came together to offer help. Initially, this came in the form of individual efforts, but quickly became organised in the shape of formal campaigns that aimed to provide medical supplies and consumables, as well as clinical expertise and hands-on support. In addition, numerous and sustained advocacy and lobbying campaigns were launched to draw the attention of the international community to the abhorrent practice of targeting healthcare facilities, in the hope that it can be forced to stop.
Importantly, the medical expatriate community recognised the immense training needs for healthcare staff on the ground, and concerted and focused efforts were mobilised to address these training issues. Relevant and useful courses were designed and implemented and training was delivered by expert clinicians and educators. Some were of Syrian descent, but many were Western colleagues whose expertise was sought and who were more than happy to share their knowledge, skills and expertise – be that to treat patients in hospitals and healthcare centres or to train healthcare staff and help them gain the knowledge and expertise they need to deal with complex war injuries.
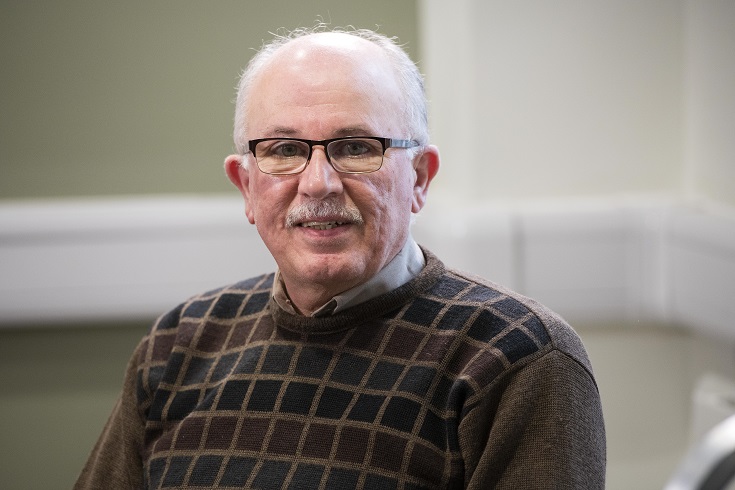
With a wealth of experience in acute care medicine, Ayman Jundi is the ideal person to lead UCLan's new postgraduate course in Disaster Medicine. He strongly believes that to do the best we can for the casualties of a major incident, it is vital to ensure that efficient healthcare systems are in place and that staff are properly trained to use them in the field. Photo: UCLan
Fast-forward again. It is 2019, and this aging warrior is yearning for some quiet times. After nearly 40 years in the practice of medicine, almost all of it on the frontline of acute care, I am looking at the option of retirement. I decided to go part-time – 66 per cent of whole-time equivalent (WTE) – at the Emergency Department, focusing almost entirely on clinical commitments.
At the same time, an interesting and attractive opportunity came up. The University of Central Lancashire (UCLan) advertised a post for a Clinical Senior Lecturer to lead and develop a master’s course in Disaster Medicine. The post is advertised as part time at 50 per cent WTE. It was the ideal progression for me – an opportunity to tap into my academic interests and share my experience in this field with the bright minds of today’s clinicians and healthcare professionals. So, I applied and I was fortunate enough to be offered the job. I’m excited about the prospect of this, notwithstanding the fact that I am now working 116 per cent WTE... some retirement!
The MSc Disaster Medicine is planned to launch in September 2020. The course will offer an exciting opportunity for interested healthcare professionals to develop the required knowledge and skills to be part of a medical relief response in case of a disaster, whether locally, nationally or internationally. It will cover a whole host of potential scenarios, from natural events such as earthquakes, flooding, and hurricanes, to epidemics and pandemics, to ‘man-made’ disasters like transport accidents and industrial events, to wars, conflicts and acts of terrorism.
The course will major on the important links to humanitarian medicine, and will offer important insight into the valuable impact of training and capacity building amongst healthcare staff on the ground, an investment that will long outlive the presence of external relief teams on the ground, leaving a true legacy of lasting knowledge, expertise and preparedness.
Find out more about studying MSc Disaster Medicine at the University of Central Lancashire.
UCLan’s School of Medicine offers a range of postgraduate and professional programmes, for the full portfolio visit their website here.
Ayman Jundi, 30/04/2020